Danger Points and Pitfalls in ProximalTibia Fracture Surgery
Danger Points and Pitfalls in ProximalTibia Fracture Surgery
Proximal tibia fractures are challenginginjuries that demand meticulous surgical management to achieve optimaloutcomes. This article highlights crucial danger points and potential pitfallsassociated with various surgical techniques, providing valuable insights foryoung orthopedic surgeons.
Infrapatellar Intramedullary Nailing:
1. Missed Tibial Tubercle Fracture:
· Danger:
Tibial tuberclefractures often accompany proximal tibia fractures. These can be easilyoverlooked, particularly in the setting of a high-energy mechanism.
· Pitfall:
Nailing alone maynot provide adequate stability for a tibial tubercle fracture, leading tonon-union or displacement.
· Recommendation: Conductthorough preoperative imaging to identify any associated tibial tuberclefractures. Consider alternative fixation methods like tension band wiring orplate fixation in conjunction with nailing for these cases.
2. Inadequate Reduction:
· Danger:
Failure to achieveanatomical reduction before nailing can result in malunion and compromised kneefunction.
· Pitfall:
Focusing solelyon restoring the mechanical axis while neglecting articular congruity.
· Recommendation:
Utilizeintraoperative fluoroscopy to confirm alignment in both anteroposterior andlateral planes. Pay particular attention to restoring articular step-offs andcondylar widening. Employ indirect reduction techniques and consider temporaryexternal fixation to aid in achieving an optimal reduction.
3. Medial Start Point:
· Danger:
Starting the nailmedially increases the risk of iatrogenic valgus malalignment.
· Pitfall:
Inadequateunderstanding of tibial anatomy and nail starting point.
· Recommendation:
Aim for astarting point slightly lateral to the center of the tibial tubercle. Thistrajectory helps maintain alignment and reduces valgus forces.
4. Distal Anterior Cortex Perforation:
· Danger:
The anterior bowof the tibia, particularly pronounced in elderly patients, predisposes todistal cortical perforation during nail insertion.
· Pitfall:
Forcing the naildespite resistance or using a nail with an excessively sharp bend.
· Recommendation:
Choose anail with a proximal or gradual Herzog bend. Monitor the nail tip's progressionwith fluoroscopy throughout the insertion. If resistance is encountered,consider upsizing the nail or utilizing a more flexible nail design.
Suprapatellar Intramedullary Nailing:
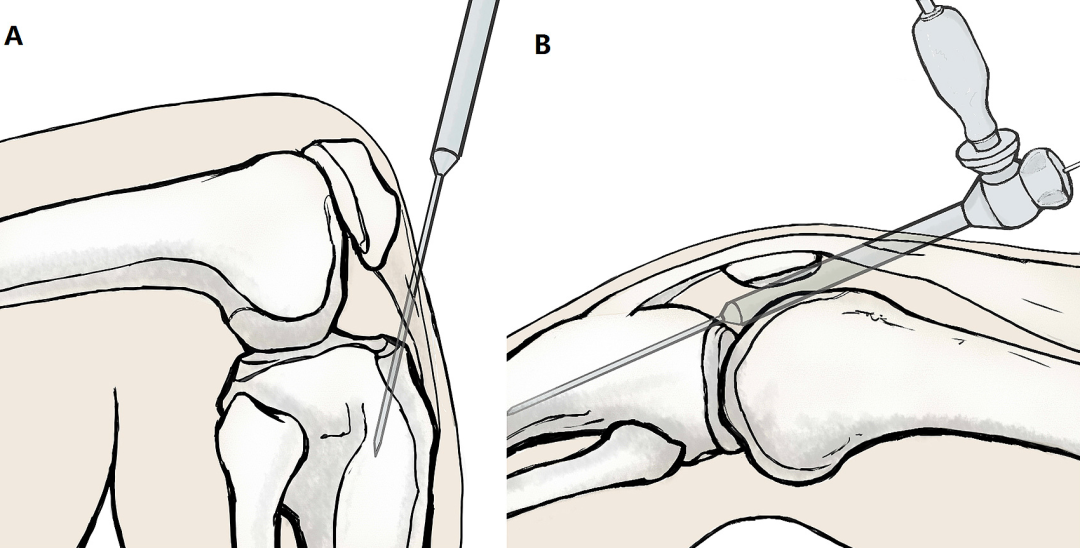
1. Tight Patellofemoral Joint:
· Danger:
A tight jointmakes cannula insertion challenging and raises the risk of cartilage injury.
· Pitfall: Forcefulinsertion of the cannula despite resistance.
· Recommendation: Assesspatellofemoral joint mobility preoperatively. Perform a lateral retinacularrelease if necessary to facilitate cannula placement and reduce stress on thearticular cartilage.
2. Cartilage Damage:
· Danger:
Direct trauma tothe patellofemoral articular cartilage during cannula insertion or reaming canlead to long-term chondral defects and osteoarthritis.
在插入或扩孔过程中对髌股关节软骨的直接创伤可能导致长期的软骨缺损和骨关节炎。
· Pitfall: Inadequatevisualization or protection of the articular surface.
· Recommendation: Use adedicated soft-tissue protector for the reamer to shield the patellarcartilage. Maintain constant visualization with fluoroscopy to ensure safeinstrument passage.
3. Inadequate Guidewire Placement:
· Danger:
Inaccurateguidewire positioning within the tibial canal can result in eccentric reamingand subsequent malreduction.
· Pitfall:
Relying solely onfluoroscopy without tactile confirmation of guidewire placement.
· Recommendation:
Use bothfluoroscopic and tactile feedback to verify central guidewire placement withinthe tibial canal. Ensure free rotation of the guidewire before initiatingreaming.
4. Malreduction:
· Danger:
Similar toinfrapatellar nailing, inadequate reduction prior to reaming and nail insertioncompromises fracture healing and knee function.
· Pitfall:
Failing toaddress rotational deformities or assuming that suprapatellar nailinginherently corrects alignment.
· Recommendation:
Meticulouslyreduce the fracture before proceeding with suprapatellar nailing. Confirmappropriate alignment with intraoperative fluoroscopy in both planes.
Spanning + Definitive External Fixation:
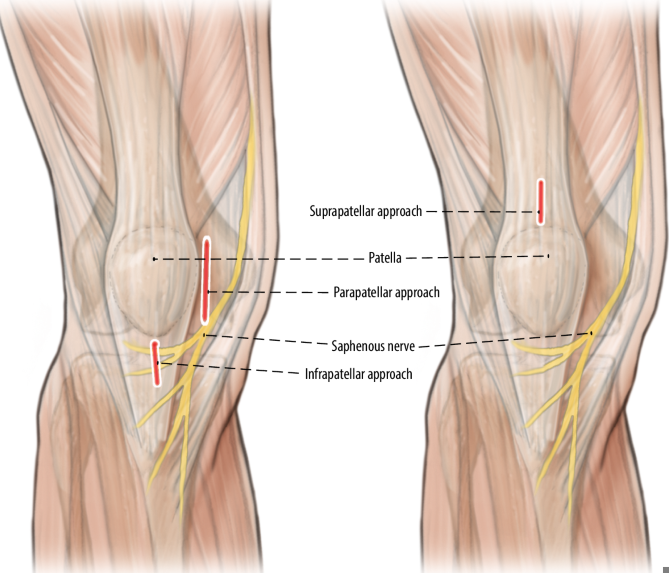
1. Pin Site Placement:
· Danger:
Improper pinplacement can damage neurovascular structures, injure the knee joint capsule,or interfere with future surgical approaches for definitive fixation.
· Pitfall: Inadequateplanning and understanding of regional anatomy.
· Recommendation: Carefullyplan pin trajectories based on preoperative imaging. Avoid placing pins withinthe zone of injury, near the knee joint capsule, or in the path of plannedfuture incisions.
2. Pin Site Infection:
· Danger: Pin siteinfections are a common complication of external fixation, potentially leadingto osteomyelitis or requiring frame removal.
· Pitfall:Breaching steriletechnique during pin insertion or neglecting pin site care.
· Recommendation:Employmeticulous sterile technique during pin insertion. Implement a rigorous pinsite care protocol with daily cleaning and dressing changes. Educate patientson signs of infection and the importance of maintaining pin site hygiene.
3. Loss of Reduction:
· Danger: Gradualdisplacement of the fracture fragments can occur over time, jeopardizingfracture healing and alignment.
· Pitfall: Insufficientframe stability or inadequate monitoring of reduction.
· Recommendation: Regularlyassess the fracture reduction with clinical and radiographic examinations.Adjust the frame as needed to maintain alignment and length. Utilize additionalfixation techniques like percutaneous pinning or minimally invasive plating toenhance stability if necessary.
4. Iatrogenic Joint Stiffness:
· Danger: Prolongedimmobilization or restricted range of motion can lead to knee joint stiffnessand functional limitations.
· Pitfall: Delayingmobilization or assuming that external fixation inherently prevents jointstiffness.
· Recommendation
Initiateearly passive and active range of motion exercises as soon as soft tissuehealing permits. Encourage patient participation in a comprehensiverehabilitation program to optimize joint mobility and functional recovery.
Conclusion:
Proximal tibia fracture surgery presentsseveral potential pitfalls that can compromise patient outcomes. Youngorthopedic surgeons must be aware of these challenges and adopt meticuloussurgical techniques, thorough preoperative planning, and careful postoperativemonitoring to minimize complications and achieve optimal results for theirpatients.
This article is intended as a guide forlearning and reference. It does not replace comprehensive surgical training orthe need for individualized decision-making based on each patient's uniquecircumstances.